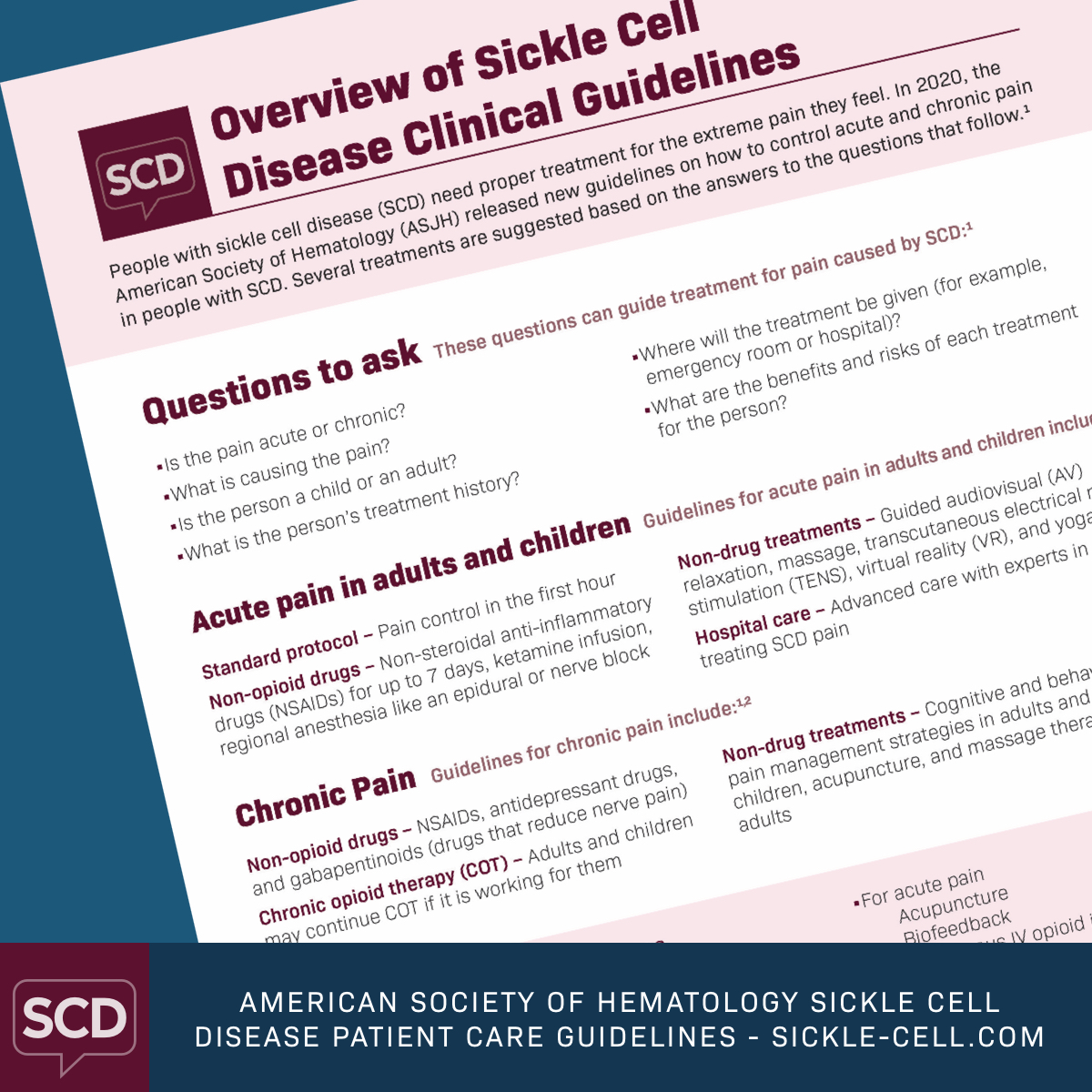
American Society of Hematology Sickle Cell Patient Care Guidelines
People with sickle cell disease (SCD) often have a lot of pain. SCD pain can happen suddenly and be severe, or it can be long-term or chronic. Pain is a long-lasting problem for those with SCD, and managing it can be hard at times.
In 2020, the American Society of Hematology (ASH) released new guidelines on how to help control acute and chronic pain in people with SCD. The guidelines contain different pain management options such as opioids, non-opioid drugs, and non-drug treatments. These guidelines can help inform your choice of the best care for you.
Drugs for acute pain
Drugs are the most common treatment option for acute pain in adults and children with SCD. The ASH suggests that people with SCD get pain relievers within 60 minutes of seeking care for acute pain.1
Non-opioid drugs are also an option for acute pain. The ASH suggests non-steroidal anti-inflammatory drugs (NSAIDs) for adults and children. NSAIDs may be used for up to a week. If the pain persists and does not respond to opioids, subanesthetic (pain-relieving) ketamine infusion and regional anesthesia may be used.1
The ASH suggests not using chronic transfusion therapy for acute pain in adults and children. Due to a lack of data, the group did not advise on the use of several drugs, including continuous opioid infusion, steroids, and IV fluids.1
Non-drug treatments for acute pain
Some people prefer to use non-drug treatments to help manage pain. The ASH suggests several options for adults and children with acute pain from SCD. These include:1
- Guided audiovisual (AV) relaxation
- Massage
- Transcutaneous electrical nerve stimulation (TENS)
- Virtual reality (VR)
- Yoga
The group did not find enough data to support a suggestion on acupuncture or biofeedback.1
Hospital care for acute pain
Sometimes a person with SCD must be admitted to the hospital due to sudden severe pain. In these instances, the ASH suggests a facility with medical staff who are skilled in providing care for people with SCD.1
Drugs for chronic pain
Drugs are also standard treatment for chronic pain in people with SCD. Which drug depends on the person’s age, the cause of the pain, and treatment history. Drugs for general chronic or nerve-type pain include:1
- NSAIDs
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Tricyclic antidepressants
- Gabapentinoids for general chronic or nerve-type pain
Adults and children on chronic opioid therapy may keep up with this treatment if it is working for them.1
Non-drug treatments for chronic pain
For those who prefer to use non-drug treatments for chronic pain, the ASH suggests a few options. Adults and children can benefit from cognitive behavioral therapy. This type of treatment helps people think in new ways to better cope with extreme pain.1
Two other suggestions for adults include acupuncture and massage therapy. While some may wonder about exercise as a treatment for chronic pain, the group did not advise on this.1
Benefits of the right treatments
The proper pain treatment can help people in several ways. If a person gets the best treatment upfront, they will be less likely to take drugs they do not need. Adequate pain management can lead to fewer care visits and no or shorter hospital stays. What is more, when pain is under control, people with SCD have a better outlook and quality of life.1
Pain treatment varies from person to person. This summary of the guidelines from the ASH provides a framework for you and the doctors involved in your care. Plus, each of the original approaches contains thorough remarks to help you weigh the benefits and risks and decide what treatment is best for you.
Join the conversation