Bone Marrow Transplant for Sickle Cell Disease
Reviewed by: HU Medical Review Board | Last reviewed: May 2025 | Last updated: January 2026
The only cure for sickle cell disease (SCD) is a bone marrow or stem cell transplant. This is a procedure where your own bone marrow stem cells are replaced by a donor’s. The new healthy stem cells produce normal red blood cells instead of sickle cells.
Very few people with SCD undergo this procedure because it is too risky. Only children with severe SCD complications who have a closely matched relative can receive a transplant. The procedure is riskier in adults and when the donor is not well-matched.
What is a bone marrow or stem cell transplant?
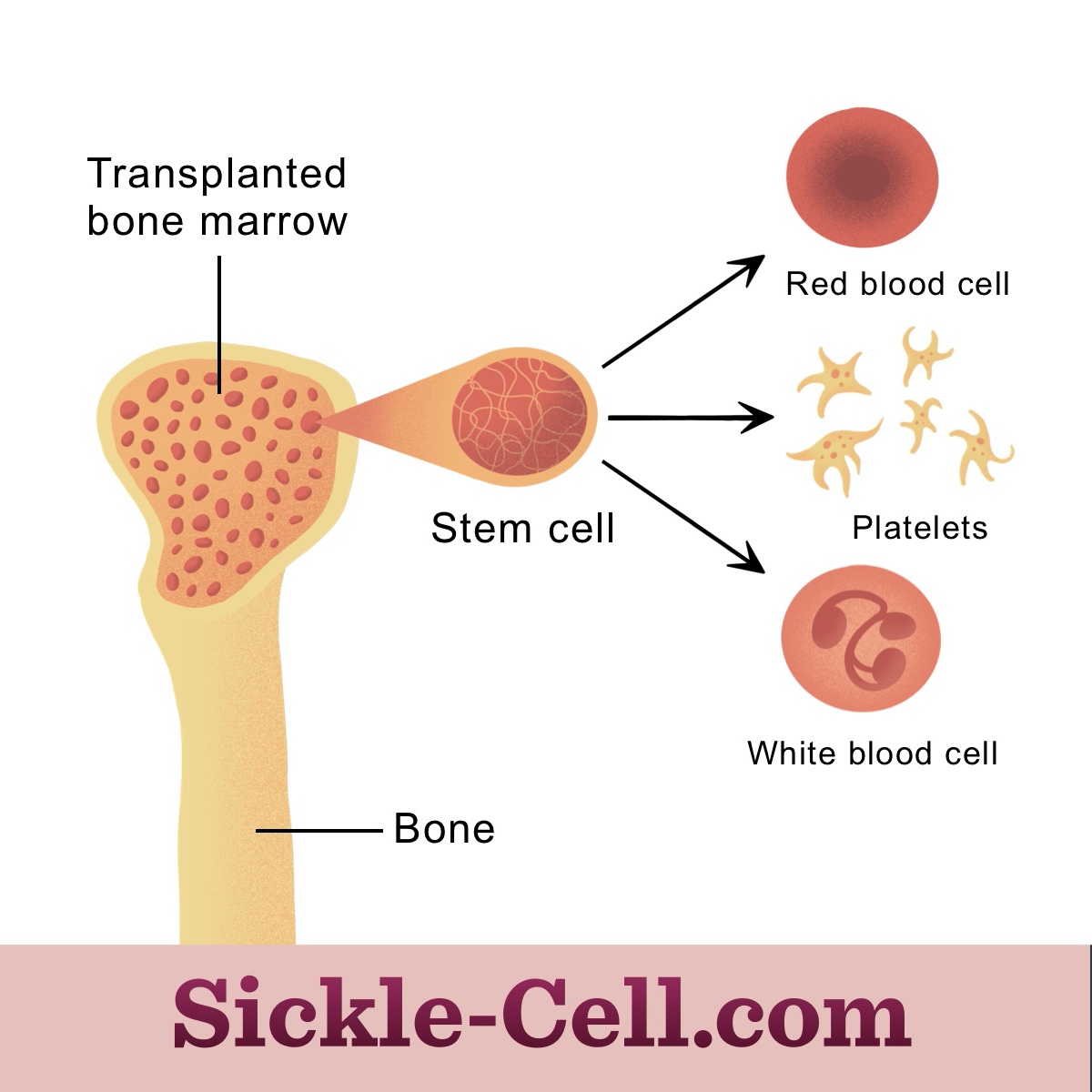
Bone marrow is the spongy center of bones that produces blood cells. Stem cells in the bone marrow produce red blood cells, white blood cells, and platelets. Bone marrow stem cells in people with SCD produce abnormal sickle red blood cells.1
A transplant of bone marrow stem cells is the only known cure for SCD. In this procedure, doctors give strong chemotherapy to remove all your bone marrow, then infuse healthy donor bone marrow stem cells to replace yours.2
Figure 1: Bone marrow transplant allows for the production of healthy blood cells
Before the transplant, your doctor will perform tests and procedures to ensure you or your child is healthy enough for the procedure. Then, they will give chemotherapy to remove the abnormal bone marrow. This will also help prevent new transplanted cells from being rejected by the recipient's cells. Then, doctors infuse healthy bone marrow stem cells into the body.2
The new stem cells then travel to the bone marrow, where they multiply and make new healthy red blood cells.
How do they cure SCD?
Bone marrow transplants are rarely performed. This is because most people with SCD are too old for a transplant or do not have a relative who can be a donor. Only about 2,000 people with sickle cell anemia have undergone bone marrow transplants.3,4
The type of bone marrow transplant used in SCD is called an “allogeneic” bone marrow transplant. This means that the healthy bone marrow stem cells come from a donor. The donor must be a family member (usually a brother or sister) who does not have SCD. The family member must also have closely matching bone marrow.2
Most transplants are performed in children. Your child may be a candidate for a bone marrow transplant if they have:1
- Severe complications such as stroke, frequent pain episodes, or frequent acute chest syndrome episodes
- Have a brother or sister who does not have SCD and has closely matching bone marrow
Talk to your doctor to discuss whether this procedure is possible or appropriate for you or your child.
What can I expect during and after the procedure?
The transplant infusion procedure is painless. Your child will be awake during the procedure. It usually then takes several weeks for the red blood cell count to return to normal. During this time, your doctor will perform frequent blood tests to ensure the new bone marrow is working properly. Additional medicines can help manage complications of the transplant.2
After the transplant, you or your child may stay in the hospital for weeks to months. The length of time depends on whether any complications occur. You or your child may also need periodic, lifelong appointments to monitor any complications.2
What are the risks of a bone marrow transplant?
Bone marrow transplants are risky in adults and with less well-matched donors. However, they are successful in about 90 percent of children when the donor is related and matched. Even with this high success rate, there are risks. About 5 percent of people who have received this procedure have died. Other risks include:1,2,4-6
- Severe infections
- Seizures
- Severe bleeding
- Organ damage
- Graft-versus-host disease (when new transplanted cells damage your own healthy cells)
- Transplant failure
Graft-versus-host disease (GVHD) occurs in about 14 percent of cases, and the transplant fails in about 2 percent of cases. These rates are decreasing as new techniques work better. Your doctor may prescribe drugs that help prevent GVHD.5,6
There are also risks from the pre-transplant chemotherapy procedure. These include:2
- Nausea and vomiting
- Diarrhea
- Hair loss
- Mouth sores or ulcers
- Infections
- Bleeding
- Anemia
- Fatigue
- Organ damage
Your doctor may prescribe drugs to reduce these side effects. Talk to your doctor if you notice any changes in symptoms following these procedures.
What is being done to expand access to transplants?
Several medical centers are researching new ways to help more people get a bone marrow transplant. This includes:4,7
- Techniques to use blood from a donor who is unrelated but closely matched
- Techniques to use blood from a donor who does not have perfectly matched bone marrow
- Techniques to cure older children and adults
For now, these techniques are too risky to perform. With ongoing research, new techniques may help expand access to this cure.8